| Michael O. Hughes, M.S.
Department of Ophthalmology
University of Virginia, Charlottesville, VA
Craig A. Luce, MSMI
Atlanta, GA and
Charlottesville, VA
In “Depicting the Anterior Eye in Two and Three Dimensions;
Part One: Cornea and Pupil,” we discussed how knowledge and artistry
are used to replicate the anterior human eye in medical illustrations
and ocular prosthetics. In Part One and Part Two the authors share their
experience and insight into the subtleties of duplicating the eyeball—accurately
and aesthetically. Part Two concludes the discussion by analyzing the
anatomical and pictorial intricacies of the iris, limbus, and sclera.
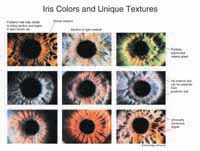
Figure 1.
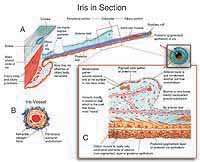
Figure 2.
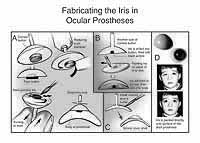
Figure 3.
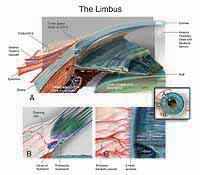
Figure 4.
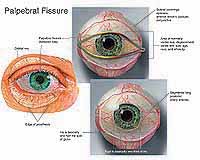
Figure 5.
|
The Iris
The human iris ranges in size from 11-13 mm. How much of this diameter
is visible to the viewer is determined by the clarity of the cornea at
the limbus, the rim of transitional tissue where the transparent cornea
joins the white opaque sclera. Though the anatomical iris is round, the
visible iris is slightly ovoid, with the top and bottom somewhat covered
by the limbus. This ovoid appearance is more pronounced at the bottom
of the cornea and in older eyes (Warwick, 1976). This “arcus senilis”
is an opaque, grayish ring at the periphery of the cornea. The artist
should remember that the limbus is in front of the iris and casts a shadow
on it, as does the eyelid.
Anatomically, the iris is generally conical in shape, defined by the lens
that pushes the central portion of the iris slightly forward. This feature
is often misunderstood, as evidenced by illustrations that show it floating
independently. Ocularists generally use the optical qualities of the prosthetic
cornea to give the artificial iris a natural-appearing, conical shape.
This shape affects the way light strikes the surface of the iris. In illustration,
light is typically depicted as coming from the upper left; thus, a painting
or drawing of the eye will show more of the upper right iris in light.
The iris best displays its three-dimensionality under biomicroscopy at
a magnification of 40X (Daughman, 1999). The thickest portion is at the
collarette, while the pupillary margin and iris root are the thinnest
areas. The sphincter muscle in the pupillary portion gathers the iris,
producing radial striations, while the discontinuous, circumferential
folds in the iris’ peripheral portion are due to the action of dilator
muscle. These peripheral folds are neither continuous nor perfect circles
(Daughman, 1999) (Figure 1).
Creation of illustrations and prostheses that look realistic requires
a nuanced understanding of eye anatomy; for example, an understanding
of what gives the anterior and posterior layers their distinctive appearance.
In a healthy human eye, it is the discontinuity of the anterior iris layer
that makes the posterior layer visible. This posterior layer gives a spoke-like
appearance to the pupillary iris, and it can be seen in iris crypts in
the periphery of the iris as well as in the varied texture of the iris
near the pupil. While only the effects of the dilator muscle’s action
are visible, the pupillary sphincter itself may be visible as a light
pinkish band (0.5 mm – 0.8 mm wide) near the pupil. It is actually
floating free in the posterior stroma, much of which is colorless and
transparent.
While peripheral iris crypts are usually covered by the limbus, and thus
unremarkable in themselves, the ciliary nature of the posterior layer
is highly evident in the pupillary region. The vessels of the iris are
covered by a thickened lamina propria and fibroblasts, and they are surrounded
by melanocytes and collagen fibrils.
The thickness of the delicate, sponge-like iris stroma is often under
appreciated, as the unpigmented portions are optically clear. Light refraction
within the walls of the iris vessels, set against the dark brown pigment
of the posterior iris’ pigment layer, creates the apparent variation
in coloring seen in light irises. A thinly pigmented iris appears blue,
while a thin stroma allows coloration to appear from the brown pigment
of the posterior iris, creating green or hazel eyes; the anterior layer
of a highly pigmented iris appears velvety brown. The absence of iris
pigment reveals the retinal reflex, resulting in apparent pink eyes associated
with albinism (Figure 2).
The identifiable elements in an individual eye include landmarks even
more unique than fingerprints and useful to computer identification systems.
For example, irregularities in the anterior layer of the iris make the
distinctive folds and furrows of the posterior layer evident. Aggregates
of melanocytes appear as brown spot nevi, while clump cells can be seen
as spherical brown spots in the peripheral stroma and near the sphincter
muscle. While a dusting of xanthin yellow pigment, or Wolffian spots,
can sometimes be seen on the surface of an eye with a light iris, almost
all the color in the iris comes from brown melanin granules in melanocytes.
The more concentrated their distribution, the darker the eye will appear.
Awareness of these highly individualized variations is especially important
for the ocularist who is creating a prosthesis to match a patient’s
fellow eye.
While there are many techniques for painting the iris, back-painting directly
onto a corneal button gives ocularists the flexibility to assemble the
anatomical elements in a variety of ways. The pupil is often preset, but
it can also be modified to an average (3 mm) size. Yellow, or another
hazy anterior iris color, is laid in as a first coat. The finest detail
of the pupillary iris can be created by scraping back the darker background
color with a blade, then overpainting the area with color variants. Nevi
can be painted first, or else drilled out of the corneal button and back-filled.
Using the brush in a scrubbing motion creates complex iris stria in the
pupillary region. These backpainting techniques have been developed for
ocularists working with traditional media. The fastest production and
drying are achieved by painting in layers with an acrylic paint and monomer
used as the catalyst. The stem of the prosthesis can be rotated to expedite
coverage (Figure 3).
In choosing iris color, medical illustrators should remember that although
the majority of human eyes are brown, choosing blue or green for the iris
will help balance the red of surgery and the black and orange of the eye’s
interior.
In medical illustration as well as ocularistry, a bit of dabbing or dabbling
with the brush can make the iris stroma appear more natural. The artist
can make tentative “scoops” of stria by scribbling with the
brush or pencil, then selectively darkening some lines. The webbing can
be made to appear more three-dimensional by painting or drawing neighboring
vessels that appear to be both “over” and “under”
the stria. Finally, while some vessel stria are corkscrew-shaped (allowing
them to straighten much like an old-fashioned telephone cord as the pupil
contracts), overemphasizing this can be distracting—the feature
is more rare than generally seen in illustrations.
Depicting the collarette “wreath” is another area that warrants
careful attention to detail. It can appear almost hazy or translucent
in the lighter eye, though often very well-defined in the brown eye. It
is scalloped mostly peripherally, like the incomplete vessel arcade it
was in the womb, and may be thought of for illustration purposes as “retreating,”
trailing strands behind it. One pitfall for illustrators to avoid is painting
the collarette as if it were simply a mirror image of the posterior stroma.
Matching a fellow eye helps ocularists create a realistic representation
of the collarette. Even though the collarette in the living eye has been
altered by disease or surgery, some ocularists create a prosthesis that
indicates a healthy collarette. Even when the fellow eye's collarette
is not well-defined, painting one on the prosthesis can soften the appearance
of the artificial pupil.
The Limbus
A natural-appearing limbus is essential in both illustration and ocularistry,
or the iris will appear unrealistically sharp and clear. Ocularists speak
of creating a “soft” or a “hard” limbus. In illustration,
this junction may be given a soft blue tint. Most ocularists produce limbal
shading, by grinding away the sclera acrylic material to a featheredge
and/or painting it.
Highlights on the transparent cornea can diffusely illuminate the side
of the iris furthest from the viewer, as well as the sclera at the limbus.
This illumination is evident in the best portraiture and illustration.
Illustrators should create a diffuse, warm glow in this area, bounded
posteriorly by the iris root. Living tissue is rarely opaque, and this
glow may be compared to the subsurface scattering of light in the skin.
The Sclera and Its Coverings
The normally near-white sclera extends from the limbus to cover the rest
of the globe. The scleral coverings (sclera, episclera, anterior Tenon’s
capsule, and conjunctiva) are virtually transparent and fuse to the cornea
near the limbus. These structures are noteworthy for ocularists and illustrators,
only in that the blood vessels seen on the white scleral surface actually
reside between these various layers and thus above the sclera itself.
Long, posterior ciliary arteries supply each quadrant of the anterior
eye and are visible in the conjunctiva. For illustration purposes, they
should not be drawn as crossing each other in the same tissue layer. The
straighter vessels of the anterior eye are arterioles, and may be depicted
as redder than veins; wavy vessels are usually veins and are larger and
generally deeper in the tissue layers than the arteriolar supply in the
same quadrant. Extremely fine vessel arcades can be seen in the region
of the limbus, just outside the clear corneal margin. Such accurate reproduction
of vascular anatomy is important for those creating both illustrations
and prostheses. In ocularistry, the effect of vessels overlying the sclera
can be reproduced by using oils and dry pigments, making vessels out of
silk threads or tracings of red pencil onto a clear covering layer, then
adding a clear coating on top of them.
If the scleral vessels are drawn or painted without an accompanying shadow,
they appear to rest directly on or in the sclera rather than above its
surface. It may be easier to reproduce the shadows first, then illustrate
the vessels. In Photoshop™, the vessels may be duplicated on a second
layer, desaturated as a multiplier shadow, and Gaussian-blurred; or, a
drop shadow may be employed to give a layered effect. The larger episcleral
or conjunctival vessels will sometimes express the external contour of
the conjunctiva and thus make two highlights possible—one just on
the vessel and another just above it, representing the reflection from
the clear conjunctival covering (Figure 4).
As is evident from the portion visible in the open eye, the sclera is
highly vascularized, more so in the portion visible between the lids called
the palpebral fissure. Color variations and nevi are seen here, for the
simple reason that atmospheric pressure on the surface of the eye is less
than that inside the globe, allowing pigment to “float” to
the ocular surface. Dark brown eyes, for example, often show a smattering
of brown throughout the sclera, most marked in the limbal and conjunctival
regions. The illustrator, and the ocularist, should be mindful of the
slight scleral yellowing, from deposited hepatic by-products that often
accompanies the aging process. This explains why “clear eyes”
are often associated with youth. The scleras of infants, or of patients
with osteogenita imperfecta, often have a slight bluish cast due to the
thinness of the sclera. The expression “baby-blue eyes” can
thus refer to more than the iris (Jakobiec, 1982) (Figure 5).
Parts I and II of this article have described the combination of accuracy
and artistry necessary to depict the anatomy of the anterior eye. More
studies on how to portray the eye’s visible portion, with attention
to the contributions of both ocularists and medical illustrators specializing
in ophthalmology, are worth undertaking. Professional collaboration and
cooperation between the fields of medical illustration and ocularistry
have a long history. The similar technical and artistic challenges encountered
by ocularists and medical illustrators are worth exploring.
Acknowledgements
For their critiques, review, and encouragement, the authors thank Howard
Bartner, Chief of Medical Illustration (Ret.), National Institutes of
Health, Bethesda, Md.; Ranice W. Crosby, Associate Professor of Art as
Applied to Medicine, Johns Hopkins University School of Medicine, Baltimore,
Md.; Sara A. Kaltreider, M.D., Department of Ophthalmology, University
of Virginia, Charlottesville, Va.; and ocularist Joseph LeGrand, LeGrand
Associates, Philadelphia, Pa. The authors also thank Victor Weaver (www.victorweaver.com)
for graphic design and Genevieve J. Long, Ph.D., Portland, Ore., for writing
and editing assistance.
References
Daughman, J. 1999. Biometric decision landscapes. Cambridge:
University of Cambridge Computer Laboratory, Technical Report No. TR482.
Warwick, Roger, ed. 1976. Eugene Wolff’s Anatomy of the Eye
and Orbit. 7th ed. Philadelphia: W. B. Saunders Co.
Authors
Michael O. Hughes is an ocularist
who has been in private practice for more than twenty years in suburban
Washington, D.C. (Vienna, Va). He is also the primary ocularist for the
Department of Ophthalmology, University of Virginia, Charlottesville.
Information on Hughes can be found at: www.artificialeyeclinic.com.
Craig A. Luce is a medical illustrator working in Atlanta and Charlottesville,
Va. He has painted ophthalmic anatomy and surgery for 28 years. Among
his work are 75 images for The Ciba Collection of Medical Illustrations,
Vol. 8, Part III. Information on Luce can be found at www.medical-illustration.com.
The authors have collaborated on many projects at the University of Virginia,
including revisions to A Singular View: The Art of Seeing With One
Eye by the late Frank Brady.
|